Project 4:
PI: Lynn Rochester
Fellow: Rana Zia Ur Rehman
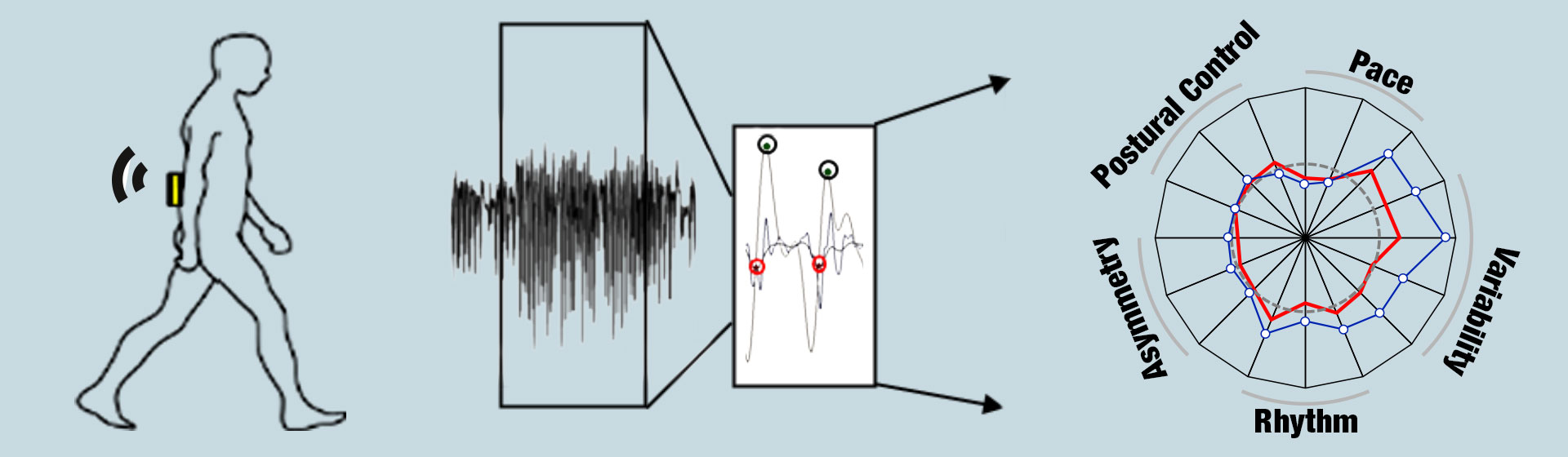
Developing novel tools from wearable sensor data for neurodegenerative disease management using deep learning techniques.
State-of-the-Art: Clinical assessment is the hallmark for diagnosis of PD and atypical Parkinsonian syndromes such as Progressive Supranuclear Palsy and Multiple Systems Atrophy. However, differential diagnosis of these Parkinsonian syndromes is challenging, and as a result patients are often misdiagnosed or experience a delay in diagnosis. For example, in a post-mortem study of 100 patients who had a clinical diagnosis of PD, histopathological features that are typical of PD (i.e., Lewy bodies) were found in only 76%. Gait and balance impairments are amongst the earliest clinical features of these conditions and may be useful to discriminate pathology in the early clinical stages of disease.
Approach: Using a model of gait that incorporates five gait domains and 16 gait characteristics, we have shown specificity of gait in early clinical PD cohorts. We will apply this knowledge to study participants with Parkinsonian syndromes in general. Furthermore, we will extend this approach to home-based monitoring which may prove to be more discriminative, and will enable integration of the ICF model. We have recently refined the use of accelerometer-based body worn monitors (incorporating novel algorithms) to quantify gait and postural control in the clinic and home and have validated this in a large cohort of PD and older adults [19], making it possible to carry out a multi-centre study. Building on this earlier work, discriminative properties of selective features of gait and postural control in the clinic and home will be assessed in Parkinsonian syndromes. We will identify accuracy for gait and postural control features alone and in conjunction with disease-specific biomarkers which provide evidence for possible and probable diagnoses.
